Baby Eczema
The chief characteristic of baby eczema is the intense itching that can become unbearable. Itching inevitably leads to scratching, increasing the chances of infection accompanied by even more itching and scratching. ScratchSleeves help to break the itch-scratch cycle by minimising the scratching damage.
What is Baby Eczema?
Eczema refers to a number of different skin conditions where the skin is red and irritated.
The skin is usually dry, but if it becomes infected then tiny blisters can form which become moist and ooze. The most common type of eczema is ‘atopic dermatitis’, also known as infantile eczema or baby eczema, although it also occurs in older children.
Baby eczema typically develops in babies between two and six-months-old, starting as a red rash on the cheeks which then spreads to the face and trunk either as patches or covering the skin.
Eczema typically flares up and then calms down, often with no obvious reason. Even between flare-ups eczema skin tends to be dry and flaky.
You aren’t alone: Infantile or baby eczema affects around 1 in 8 UK babies and children. Around two-thirds of them grow out of eczema by the time they are seven.
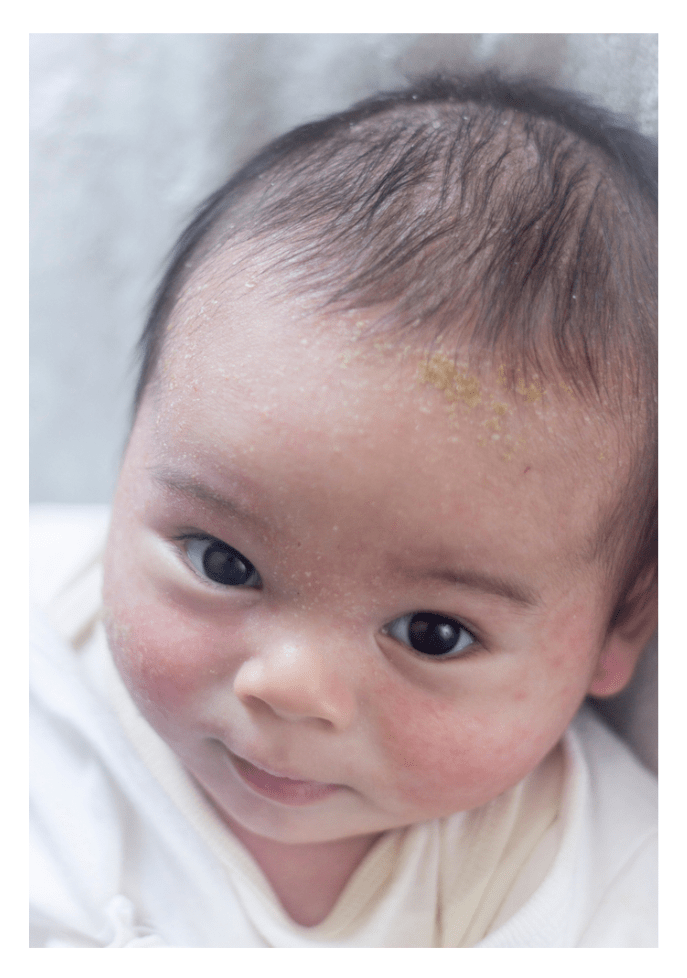
What does Baby Eczema look like?

Atopic dermatitis is the most common form of eczema and often begins during childhood. Babies with eczema will usually begin to show symptoms before they turn six months old.
Those symptoms can be slightly different in babies than in older children or adults.
Babies will usually first experience skin inflammation on their cheeks, forehead, or scalp. On light skin it will look red and may be pimply. On darker skins the inflammation can be harder to see and will often appear as darker patches.
The eczema rash may then begin to spread to the skin in the fold of the elbows or knees as the baby grows.
When babies first develop eczema, the irritated skin will often be red and weepy rather than dry and flaky. Typically, the rash then begins to dry out as the baby gets older.
As well as atopic eczema, babies may also develop other types of eczema including:
- Contact dermatitis – Eczema triggered by the skin coming into contact with a particular substance.
- Infantile seborrheic dermatitis, also known as cradle cap – Eczema on the scalp.
- Dyshidrotic eczema – Eczema on the hands and feet.
Baby Eczema and Cradle Cap symptoms
The symptoms of eczema in babies can vary depending on the age of your baby and the type of eczema that they are experiencing.
Skin irritation caused by eczema can occur anywhere on a baby’s body, and is most frequently characterised by the following symptoms:
- Patches of skin inflammation that look red or weepy
- Irritated, red, or dry patches of skin on the forehead, scalp, or cheeks
- On darker skin, an eczema rash look purple, brown, or grey
- Crusty or flaky skin on the scalp
- An eczema rash on the elbows, knees, hands, or feet
- An infected skin rash that looks yellow and crusty
Other signs that your baby may be suffering from skin irritation caused by eczema include:
- Scratching at their skin
- Disrupted sleep
- General fussiness
Cradle cap
Cradle cap is a common type of infantile seborrheic dermatitis. According to the National Eczema Society, it usually appears by the time a baby is three-months-old and typically resolves between the ages of six and twelve months.
Unlike atopic dermatitis, cradle cap does not tend to be itchy or cause any discomfort. Advice from the NHS says that it is not clear what causes cradle cap, but that it is a harmless condition that should clear up on its own.
The main symptom of cradle cap to look out for are yellow crusts of skin that may flake away to reveal red skin underneath.
Whilst cradle cap is most commonly found on a baby’s scalp, it can also appear on other parts of the body including the eyebrows, behind the ears and the nappy area.
What causes Baby Eczema (Atopic Dermatitis)?
The causes for baby eczema are unclear but it does tend to run in families, making some people genetically more susceptible to developing it.
Three quarters of atopic eczema sufferers have parents with atopic conditions such as hay fever, asthma and eczema.
According to the NHS, ‘people with atopic eczema often have very dry skin because their skin is unable to retain much moisture. This dryness may make the baby’s skin more likely to react to certain triggers, causing it to become itchy and sore.’
What can make Baby Eczema worse?
If your baby has eczema, you are likely to find they have good days and bad days with the condition.
There is no known cure for eczema, but with some trial and error it is possible to manage eczema symptoms to alleviate discomfort and soothe your baby’s skin.
You will find that there are often triggers that cause your baby to flare up and go through a rough patch with their eczema, so learning what these triggers are and working out ways to avoid them can help you to manage your baby’s eczema symptoms.
Eczema triggers are different from one baby to the next and may even change over time.
Common eczema triggers to avoid include:
- Rough or synthetic clothing materials
- Long or hot baths
- Synthetic or harsh ingredients in toiletries
- Soaps or detergents
- Becoming overheated
- Allergens (pets, pollen, dust mites, mould.
- Food allergies
- Teething
Every case of baby eczema is different, but you will usually find that there are triggers that cause flare-ups.
Identifying and avoiding the triggers for your baby’s eczema is one of the most effective ways of treating them.
However, this is easier said than done as each case of atopic dermatitis is unique.
The ScratchSleeves blog aims to cover the wider aspects of living with your child’s eczema or toddler. The things that medical professionals won’t know to tell you unless they have personal experience of living with eczema. As well as an Eczema 101 section and information about both conventional and alternative treatments, it covers practical stuff including laundry, eating well for eczema, identifying triggers and managing allergies.
How to treat Atopic Eczema in babies?
Eczema treatments aim to improve the moisture levels of the skin using emollient (moisturising) creams and topical corticosteroids (usually hydrocortisone) which are prescribed to reduce swelling and redness during flare-ups.
There are a plethora of atopic dermatitis emollients and eczema creams available both on prescription and over the counter.
In our experience, an emollient has around a 50/50 chance of being effective, so it really is a case of trial and error to find an effective treatment for your baby’s condition.
One thing to note is that moisturisers should be applied generously and smeared over the skin (in the direction of the hair growth) rather than rubbed in. This ensures that sensitive skin is not pulled and stretched unnecessarily and that sufficient moisture is supplied.
When to seek medical advice
Eczema can be itchy and uncomfortable for babies and depending on the severity of the condition it may also cause complications or have a psychological effect in the long term.
You will need to speak to your doctor when you first notice the symptoms becoming a problem or causing discomfort. You may also require further medical advice as your child grows and as the condition changes over time.
Baby eczema
If your baby has itchy rashes or irritated skin and you suspect they may have eczema, then it’s important to book an appointment with your GP to receive a diagnosis.
Your doctor will look at the rash and ask you a few simple questions to diagnose the condition.
If eczema is diagnosed your doctor should assess the severity of the condition and then help you to identify triggers and manage your baby’s symptoms.
Many of the creams and emollients used to treat your baby’s eczema are available on prescription.
Cradle cap
Cradle cap does not usually require any treatment because it shouldn’t cause babies any distress and often clears up of its own accord. It is possible to buy special cradle cap shampoos from the pharmacy to try to help the condition clear up quicker.
You may wish to seek medical advice from your GP if your baby’s cradle cap is appearing on other areas of the body as well as the scalp.
If the cradle cap begins to ooze fluid or the area of affected skin looks swollen, then the skin could be infected, and you should seek immediate help from your doctor.
Skin infections
Baby eczema can be prone to infections if the baby is frequently scratching at their irritated or broken skin with sticky or grubby fingers.
Early symptoms of skin infections include:
- Redness, warmth, or swelling around irritated skin
- Pus-filled lumps around eczema rash
- A fever
- Skin that looks blistered
If your baby experiences any symptoms of a skin infection, seek advice from your doctor immediately.
How to stop babies scratching
The intense itching of baby eczema inevitably leads to scratching.
Once the skin has been broken, the chances of bacterial infection are greatly increased (see above).
One way to stop the scratches is to keep fingers nails clean and short. However, it may also be necessary to cover the hands of babies and children who can’t stop themselves from scratching.
The unique double-layer mitts by ScratchSleeves minimise the risk of scratches, while the cool silk outer mitts is calming on the skin. The loose-fitting sleeve design ensures that the mitts stay on at the same time as avoiding any irritation of sore areas on hands and wrists that can occur when wearing conventional scratch mitts (or socks over the hands). See more information.
Keeping eczema babies clean
Keeping an eczema baby’s skin clean is essential to reduce the risk of infections. However, soap and a bubble bath can make the condition worse because they strip the skin of its natural oils as well dirt.
Hot water can also dissolve the skin’s natural oils and dry it out, so eczema children should be bathed in tepid or warm water.
Every child is different and you’ll need to find out what works for yours. Our approach is to avoid soaps and bath products altogether and use a micro-fibre wash mitt from ENJO. When the dirt is just too much, we use gentle, paraben-free toiletries.
More Information
Visit the ScratchSleeves blog and Facebook page for more information on identifying eczema triggers and living with an eczema baby. Our Childhood Eczema page also has more information.
- NHS choices – more information on diagnosis and treatment
- NSGCCE – Nottingham Support Group for Carers of Children with Eczema: a fantastic resource focused on childhood eczema
- Eczema Outreach Support – Charity founded in 2011 by a mother of an eczema child offering support for the entire family
Our Sources
- National Eczema Society – Article on Seborrhoeic dermatitis & cradle cap in infants
- Information on Cradle Cap – Provided by NHS
- Information on Atopic Eczema – Provided by NHS
Quick buy